A Mutating Virus Spreads Across America
December 10, 2021
On January 20, 2020, the United States confirmed its first case of a novel coronavirus, SARS-CoV-2. By March, the World Health Organization (WHO) declared the virus, now referred to as COVID-19, a pandemic as hospitals filled up worldwide. As humans worked to find a cure, the virus continued to mutate. Mutations were found in places such as the United Kingdom, South Africa, Brazil and quickly spread to other countries including the U.S. Humanity’s combative strategies of social distancing, quarantining and, as of late 2020, mRNA vaccines, were becoming less and less effective at slowing the spread. One of the most concerning variants, the Delta Variant, was first discovered in India in December 2020 and has spread rapidly through the United States partially due to its higher transmission rate, almost double that of the original virus.
All viruses evolve over time and undergo changes as they spread and replicate.
— Dr. Inci Yildirim
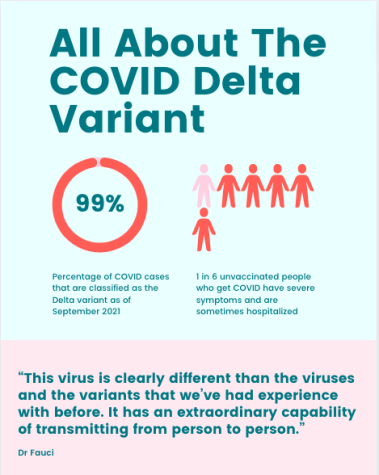
At the beginning of September 2021, the Center for Disease and Control (CDC) stated: “[the] Delta Variant accounts for more than 93 percent of all U.S. COVID-19 Cases.” Despite the fact that about 57% of the U.S. population is vaccinated, the Delta Variant continues to spread. The Pfizer-BioNTech vaccine was determined to be about 95% effective against the original SARS-CoV-2 variant. Nevertheless, officials estimate that the efficacy rate of the same vaccine is between 42% to 96% when facing the Delta Variant. Additionally, according to the CDC, while people who have already received doses of the vaccine can still contract COVID-19, those who are vaccinated have less severe symptoms, are less likely to be hospitalized, and spread the disease for a shorter period of time. According to Dr. Inci Yildirim, a Yale Medicine pediatric infectious diseases specialist and a vaccinologist, “As older age groups get vaccinated, those who are younger and unvaccinated will be at higher risk of getting COVID-19 with any variant. But Delta seems to be impacting younger age groups more than previous variants.”
So far, as COVID-19 has spread all around the world, there have been a multitude of variants. The CDC recognizes five variants as the predominant ones: Alpha, Beta, Gamma, Delta, and Omicron but only Delta and Omicron are recognized as “variants of concern.” But how come this virus is mutating so quickly? Dr. Yildirim is unsurprised by the natural mutation of the virus. “All viruses evolve over time and undergo changes as they spread and replicate,” she said.
The mechanism behind how viruses multiply is essentially finding and hijacking a host cell and making more of the virus. So, each time there is a new copy made, there are bound to be minor errors. According to National Geographic, “mutations can tweak the building blocks of proteins encoded in the DNA or RNA, which alters a protein’s final shape and prevents it from doing its intended job.” In this case with the Delta Variant, the changes are pretty large, so more precautions have to be taken.
While the Delta Variant as a whole still causes people to have relatively similar symptoms to all previous forms of COVID, the rate of transmission and vaccine efficacy are what experts are highlighting. Much like other variants, Delta spreads faster than not only the original strand of COVID-19 but also much faster than all previous variants which is what makes it so concerning. On top of that, while FDA-approved COVID vaccines still remain effective against preventing serious cases of COVID-19 in those who are fully vaccinated, if one happens to contract COVID-19 even when vaccinated (this is called a breakthrough infection), they can continue to spread the virus to others even if they themselves are asymptomatic.
While we can’t stop the virus from mutating, we can limit the spread through social distancing, wearing masks, and getting vaccinated. By limiting the spread, we reduce the chances that a mutation can develop. In an article published by Johns Hopkins University, virologist Andrew Pekosz tries to break down how this works: “Say, for example, it’s a one in a million chance that a mutation will be advantageous to the virus. If you let the virus replicate itself 900,000 times, odds are that the advantageous mutation will occur. But if you limit the overall replication of the virus to 1,000 times, then it’s much less likely that the random advantageous mutation is going to occur. And that is where public health interventions really help us a lot during this pandemic — by reducing the total amount of virus replication and therefore reducing the chances that the virus can improve or adapt.”
While no public health intervention method is perfect, each one will help to limit the spread of the virus. For more information on COVID-19 variants, visit cdc.gov.